
Hi, help us enhance your experience
Hi, help us enhance your experience
Hi, help us enhance your experience
1685 Views
Dr. Kumar Prafull Chandra, Director, Dept. of Internal Medicine & Diabetes care, Healthcity Vistaar Hospital; and, Chandra Diabetes & Obesity Clinic, Gomtinagar, Lucknow 29 August 2023
Generally, thyroid function test (TFT) interpretation is straightforward. However, in certain conditions causes unusual TFT patterns are likely. In such cases, clinical correlation is warranted.
The thyrotropin-releasing hormone is released from the hypothalamus, which catalyzes the release of thyroid-stimulating hormone (TSH) from the pituitary gland. TSH prompts the thyroid gland to release thyroid hormone, which in turn, provides negative feedback to the pituitary against TSH. Thus, thyroid release is under tight equilibrium. Relatively small changes in free-T4 cause significant TSH alterations – a sensitive parameter for measuring thyroid function.
However, in certain conditions, the feedback mechanism malfunctions, such as – central hypothyroidism, non-thyroidal illness, recently treated thyrotoxicosis, resistance to thyroid hormone, TSH secreting pituitary adenoma.
Diagnosis of thyroid dysfunction must follow:
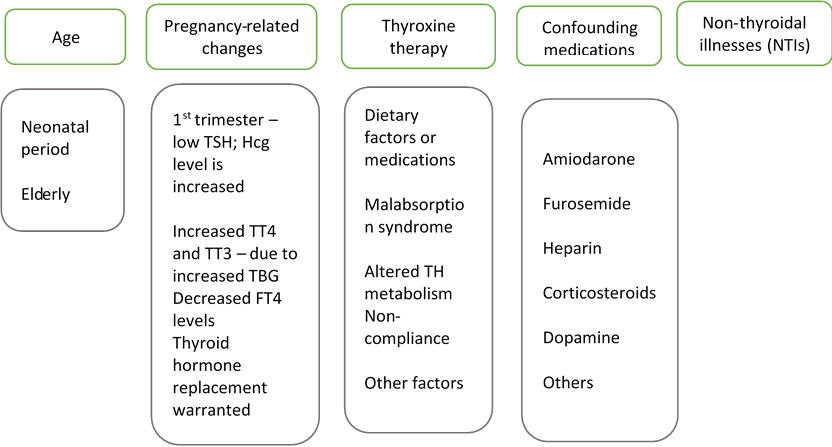
Clinical Conditions:
Euthyroid sick syndrome: Common finding after chronic illness. Pre-illness TFT is detrimental in assessing thyroid hormone replacement therapy.
Heterophilic Antibody Interference: Incidence 0.05%-6%. Heterophilic antibodies like Human Anti-Mouse (HAMA) can cause falsely elevated TSH levels.
Conditions leading to Thyroid Hormone Resistance:
Discordant TFTs – Steps to follow when Thyroid function fails to respond to the clinical scenario:
![]()
{{Article_Title}}
{{Article_Author}}
{{Article_Title}}
{{Article_Author}}